Our Results
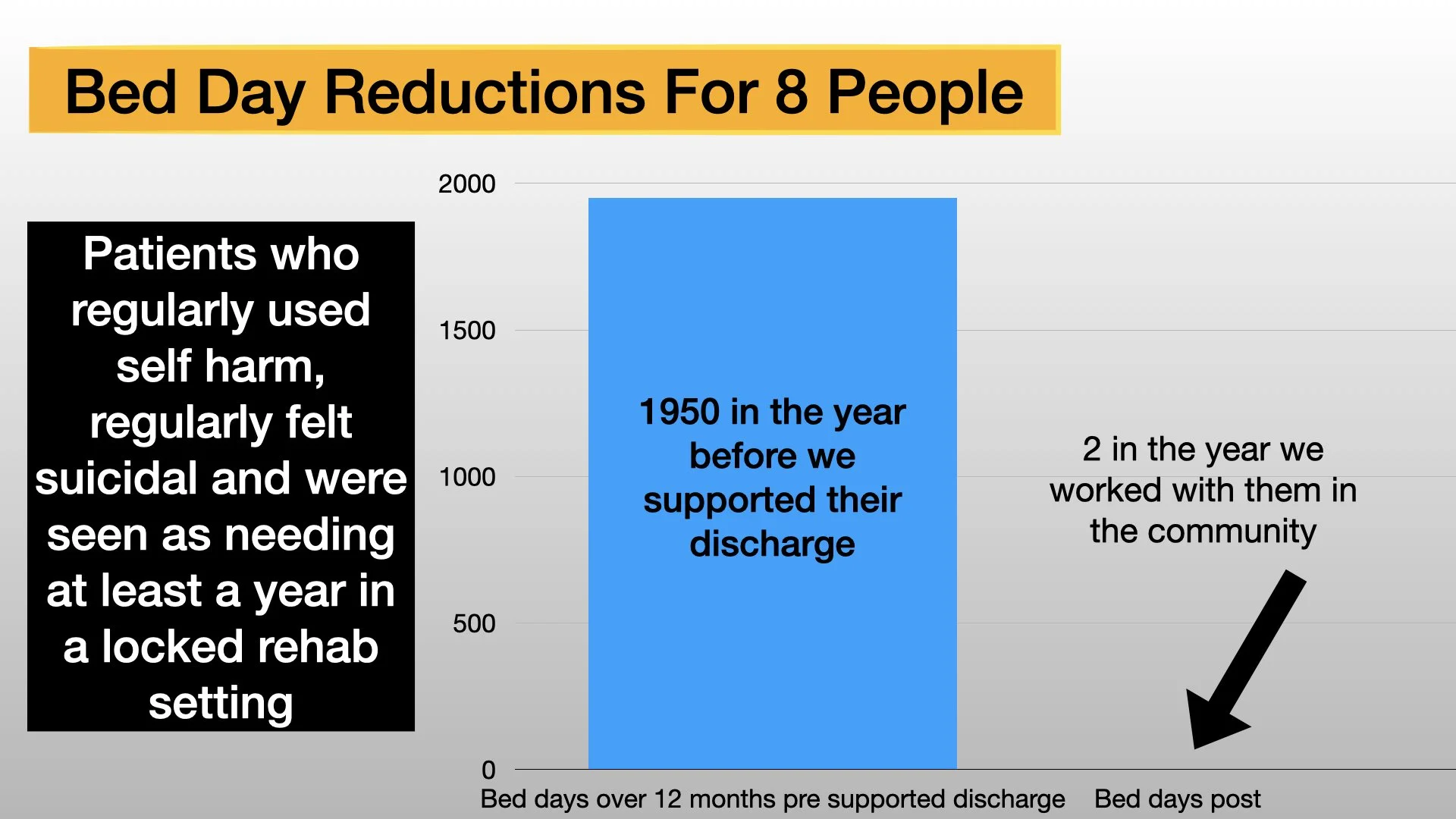
We support people who recurrently self harm and feel that life is not worth living. Often they are stuck in acute hospital wards and/or at risk of going to self declared specialist units. Below are bed days used by those that we worked with before and during our time working together. Its likely that we’ve underestimated the bed days pre our input.
What people who have worked with us say?
“Beam is a life changing support network, when all treatments have failed and this being the last resort 100% take the opportunity if you don't try you will never know! initial starts are the hardest but you will get through it! The beginning is hard as you go on you will see a massive difference. I would not be where I am today achieving my goals without their support. Determination is key! works both ways you putting in the effort to make changes to get well otherwise its pointless. BEAM are people that want the best for you and with all the expertise they sure do a good job better than actual NHS CMHT WORKERS. They’re people you can speak to at 9pm when your sat crying on a hospital bed trying to help you piece yourself together. Help you in ways hospital cannot. 100% give it a go, always, coming from someone who wanted to give up multiple times”
“For the people who are considering working with BEAM, I highly recommend it. Its taught me so much about myself and the support is extraordinary. They have been the most useful and supportive professionals in my life and have gotten me through so much. Sometimes doing a new form of therapy can be scary, but both Keir and Hollie make it fun and will help you to understand it much better. They always have your best interest in mind and will do anything they can to help. Their extended phone contact is useful if you struggle more out of working day hours and are honestly there when you need them. They keep to their promises and won't give up, and will always work with you and encourage you to be the best self you can be”
“I wish I could write something that will transform someone’s thinking and turn things around for them. If I had read a motivational and reassuring patient testimony at the height of my difficulties, I would have most likely screwed it up and thrown it away. To think there was hope outside of the toxic cycle I had found myself in seemed unrealistic, I would scoff at those motivational posters that ironically decorated the hospital walls and yet here I am trying to share the message that there IS HOPE. If this message does reach someone like me then please know that this life is worth living and things can get better if you want them to. I think the key is to want the change. As soon as you can begin to make sense of that want, and to then actualise that motivation to live a more fulfilled life then you will see such a difference. Trust in Hollie and Keir but most importantly trust in yourself.”
“As dramatic as it sounds, going to a long term placement would have stunted my life so much so that I can’t imagine ever being able to regain a normal life.
As important as hospital was in keeping me alive, the detriments it caused cannot be ignored. My self-harming behaviours escalated enormously, my independence and basic living skills withered away, I lost my interpersonal skills and confidence in relationships
”
“I was told “You mustn’t work for at least a couple of years.” “You should stay away from the pressures of work as it could contribute to your feelings of inadequacy …” “You might not be able to cope.” Not once did anyone acknowledge that I was good at my job. It was never appreciated that I had worked from the age of 12 and that I thrived off the autonomy and responsibility it gave me. No one ever considered that working was massively part of my positive self-concept and that by denying me this one thing, it was denying me the hope and optimism that things could be better and return to some new kind of normal in the world outside the ward. What I was being told simply reinforced the feelings of inadequacy and failure that I had been trying to break away from during my admission. I was devastated.
Something else I was told needed to happen was: “You must take away all the knives in the house.”… “Lock all the windows.” Wow, in retrospect I now see how unhelpful this was. I was sent home with an enormous fear of anything that could potentially cause me harm. This fear only heightened by these normal household items being hidden away. Its like the monster under the bed is for a child, the fear is in the unknown. Are they there? Will they hurt me? Again this instruction left me feeing weak and incapable. Why was I sent home with no one giving me the confidence that I could manage, being told everything I should avoid or get rid of just in order to cope day to day?
Keir and Hollie worked so hard to help me rebuild self-belief and trust that had been so badly damaged by others.
At the point of BEAM being mentioned and starting to come into the picture I had been in hospital for many months and the ward was the most unsettled and distressing it had ever been. I was physically and mentally drained, dosing up to the maximum on PRN medication, isolated from family because of COVID restrictions and using anything I could find to harm myself. I was at a point of total hopelessness and exhaustion and so I didn’t have the energy to get excited about this new service being offered to me. I was told that it was a specialist service with a phone line, a DBT program and a lived experience practitioner. I really want to say that I was excited and hopeful but I wasn’t. At this point it was just another possibility. Previous options hadn’t worked out so why would this one? And if they are as brilliant and specialist as people say they are then why on earth would they select me to receive this help? I didn’t feel deserving. In all honesty I had 0% faith that this referral would result in anything.
What was most useful and worrying at the same time was your persistence. I had become very good at getting out of difficult meetings on the ward, storming out, telling staff to fuck off and in time this meant that difficult discussions weren’t had. However, BEAM came along and would meet with me without fail. No matter the upset they would continue to come and see me which no one had ever done before. Mindfulness practice was so hard in the beginning, my intrusive thoughts would relish the opportunity to take over the second I would sit quietly and tune into them. In all honesty it felt like torture. But Keir persevered and every session we would engage in mindfulness practice without fail, so useful but equally as worrying for me in the beginning.
Choosing BEAM was a decision based on an accumulation of many factors. For wish of a better word, the ward was becoming crazier and I was finding that the time I spent with Hollie and Keir was the only hour of peace and reflection I was getting in the week. I was insight into what I could possibly have outside. Don’t get me wrong, our sessions were hard. I would get upset, cross, frustrated but that is exactly the point…It allowed me the precious time and space to be upset, cross and frustrated and to truly feel, experience and express. I gradually came to realise how precious that was and how much I anticipated our sessions. I was genuinely in awe of your knowledge and understanding which was another factor in my decision to choose BEAM. Both Hollie and Keir were able explain things in such straight forward and simple terms, things that I had battled for years to find the words to explain. This gave me a real sense of comfort and safety. Yes of course there was also a real sense of no other option. I was at a point where I’d exhausted all ways of harming myself on the ward and nothing had fixed things for me, a specialist unit wouldn’t help me and the thought of being on the ward for another year would be my worst nightmare. I’d rather die than stay in my current situation. For the first time, in possibly forever, I had professionals interested in my voice and mine alone. Until now, the wishes of my partner and family were so significant and dictated the choices I made. My first several ward rounds took place without me. To be in charge of my own therapy was a change that I didn’t realise how badly was needed and was another reason why I chose BEAM. I felt that for the first time it was something just for me.
I instantly felt an ease in Hollie’s company. She had explained that she had previously been in and out of hospital but we never discussed anything further … we didn’t need to. I knew that she knew exactly what I was going through. To sit opposite someone who had been through the same and yet was so composed, insightful and compassionate was inspiring and proved to me it was do-able. Hollie continues to be an inspiration for me.
I understood that Keir had an OT background, but I feel it was his general character that made more of a difference. Keir carries with him the most incredible aura of calm which was refreshing. So much of the time, mental health professionals present as authoritative, aloof, and clinical so to be in the company of someone with so much knowledge and yet so approachable and warm made a significant difference in me feeling able to engage. For both Hollie and Keir, their expertise in this area was so evident from the beginning purely through the language they would use. Both would help me unpick what I was thinking and help place the appropriate label to it. Their extensive emotional vocabulary specific to my difficulties and needs helped me understand what I was thinking and feeling more than ever before.
Something that really stands out would be how you were so willing to be present during my upset or panic attacks. On the ward, when feeling extremely distressed you were often left alone with instructions to “calm down”. Staff would say that someone in a real state couldn’t be reasoned with. This made me feel so abandoned and unworthy. But with Beam, Hollie and Kier would stay, talk me through a panic, allow me the time to cry.
That being said, looking back, I think meeting with you may have been what caused the change in me on the ward. By that I mean my destructive behaviour, the intensity of my anxiety attacks became less. Perhaps I didn’t need to prove that I was struggling anymore, because there were two people who “got me”, who had empathy as well as faith. Having a tangible, black and white report that detailed so many of the reasons for my struggling gave me that concrete validation I needed. It wasn’t just words spoken and then forgotten, they were down on paper in black and white which I could hold and read and by doing so allow myself that little bit of empathy I had refused myself until then.”
What staff who have worked with us say
(1) I first came across Beam consultancy when I heard Keir Harding speak at an occupational therapy and personality disorder conference. A little while after, I commenced my role in a community mental health assessment team where I worked with a client who self-harmed on a mostly daily basis, was suicidal and frequently put their life at risk.
They had many inpatient admissions and frequent contact with A&E and emergency services. There were multiple safeguarding alerts, risk panel meetings and MDT reviews with no improvement in their well-being or reduction in risks. The CMHT psychology service declined to work with her as their mental health was deemed too unstable. During one admission an out of area placement began to be discussed by the wider team. My client had not responded well to inpatient treatment and in fact rather than containing risk, their self-harming increased during their admissions. They were keen to explore other options that would enable them to receive therapeutic treatment in the community, remaining at home with their partner. Recalling Keir's seminar at the conference I decided to contact Beam for more information on their placement avoidance package.
I emailed and booked a telephone discussion to talk about my client and what Beam could potentially offer. Keir and Hollie were positive that Beam could work with my client and advised that the next step would be an assessment with them. This was extremely reassuring to hear, particularly given their prior experience of being declined for therapy.
I then contacted our local CCG to have a further discussion with the lead commissioner for mental health services regarding funding of an assessment. Not having worked with Beam before, she was eager to find out more and liaised directly with Keir and Hollie. She gave the go ahead for the assessment and recommended that I complete an application for Continuing Healthcare funding. This involved outlining the 6-week assessment offer from Beam with funding also being requested in principle for the full placement avoidance package. This was to avoid any potential funding delays if the assessment progressed to intervention. The application involved demonstrating the clinical need for the treatment and cost to health (or in this case life) of not having the treatment. Once completed I submitted to panel and had the funding approved. Throughout this process Keir and Hollie regularly checked in with us to offer any support needed with funding panel.
From here the assessment was arranged. Due to COVID restrictions this was completed via a mix of face-to-face appointments and video calls with Keir and Hollie. There were various sessions with my client, their partner and with myself and my colleague (I was joint working by this stage). This led to a very comprehensive formulation with an offer for a further 12-month intervention. Prior to the intervention commencing we convened a risk panel meeting attended by the trust's Patient Safety Lead, local CCG and CMHT managers. When convention was leaning towards a “specialist” inpatient treatment, it was important to develop a risk management plan for the proposed treatment in the community with full sign up from all those involved in their care as well as senior managers.
As part of the placement avoidance package Keir and Hollie offered twice weekly sessions with the client and access to telephone support in-between sessions should she need it. There were also formal supervision sessions for staff working with her as well as additional advice, guidance and support via email and phone calls. My client completed the 12-month intervention and during the time Beam worked with them, they had only one further brief inpatient admission which was early in the assessment phase. They remained living at home with their partner throughout her treatment.
“I have nothing but positive things to say about my experience of working with Keir and Hollie. I fully believe that they changed the course of my client's life. Having previously worked in acute inpatient services, I have seen many clients presenting with similar difficulties, being sent to out of area placements. I had not seen any clients who had benefitted. I felt that they were on the same trajectory.”
Keir and Hollie helped me to work from a place of curiosity and compassion rather than from a state of fear. Prior to Beam's involvement I had felt that my only input was firefighting and "managing" risks. Our therapeutic relationship was strengthened by Beam's support as their formulation refocused me on my client as a person rather than a "safeguarding alert" or a "client in red zone" (CMHT zoning). They were steady, calm, and reassuring and with their support and I felt that I was part of a team holding the risks together. We were able to move towards an intervention that addressed the root causes of my client's difficulties rather than a sole focus on stopping the risky behaviour. It all felt less reactive and hopeless.
On a personal level, I learnt so much from Keir and Hollie's vast knowledge and experience. This enhanced my clinical skills and has been transferable to other roles. I would highly recommend working with Beam. They are passionate in their support of their clients; they help you reflect and challenge what’s working and not working. I think the outcome for my client speaks for itself, they avoided placement with their package.
(2) “I have been working along side Beam for over a year now and the benefits are multi-faceted. Firstly, their approach to the individuals they support is flexible and validating, whilst clearly communicating about boundaries in a way that equally respects the person in receipt of their services and the Beam workers. The practice what they preach, walk the walk and apply these supportive principles to everyone they come in contact with including the statutory services they work alongside.
Strategically, they know the evidence regarding working with people will the sorts of trauma histories and resulting destructive behaviours. They are willing to share this knowledge and support services to think through how to work in a respectful and empowering way in the face of tricky relationship dynamics. We are using their work to trial out approaches so we can gain supporting evidence for adapting the NHS services in the most helpful way.”